The financial health of a multi-specialty practice hinges on one critical, often underestimated process: provider credentialing. When a new cardiologist, dermatologist, or physical therapist joins your team, their ability to see patients and generate revenue is completely frozen until they are successfully credentialed and enrolled with payers. A single misstep can lead to months of delays, creating revenue gaps that can cripple a practice’s growth. In fact, more than half of credentialing applications contain errors or missing information, making it the primary cause of onboarding bottlenecks.
For multi-specialty practices, this obstacle is even bigger. It is a tough task to handle the different requirements for various specialists spread across a number of insurance plans. This guide comes with a detailed medical credentialing checklist for 2025, explaining the main payer credentialing steps and the smart ways to become the best in provider enrollment. We will dissect the whole process, highlight the challenges faced by multi-specialty groups, and guide you on how to get a smooth, efficient workflow that will let your providers start practicing sooner. So, keep reading further!
1. What Exactly Is Medical Credentialing?
Medical credentialing is the method by which the qualifications, experience and eligibility of a healthcare provider for participating in the insurance networks are verified. For multi-specialty practices, it means verifying that each of the doctors and specialists working in the practice is approved by the respective payers.
This is a critical matter because, without proper credentialing, your practice will have problems with claim rejections, delayed payments, or even regulatory fines.
2. Difference Between Provider Credentialing and Payer Enrollment?
These two terms are often confused and before diving into the checklist it’s important to know the difference between these two related but distinct processes:
- Provider Credentialing: As discussed above, it is the process of verifying a healthcare provider’s qualifications to ensure they meet the established standards for delivering patient care.
- Payer Enrollment: This process follows credentialing and consists of formally requesting membership in a payer’s (insurance company) network. The insurance company performs its own verification to make sure that the provider is allowed to get reimbursed for the services provided to its members. Claims for services will be refused if payer enrollment is not successful.
A provider cannot be enrolled without being credentialed, and without enrollment, they cannot generate revenue from insured patients.
3. Why Credentialing is More Complex for Multi-Specialty Practices
A single-specialty practice, like an orthopedic group, encounters a fairly similar and straightforward set of credentialing and enrollment requirements, whereas multi-specialty practices face significantly higher complexity.
- Diverse Payer Requirements:
In a multi-specialty practice, different plans are required for different specialties. For instance, a dermatologist in the same practice might have to deal with different cosmetic or specialty plans, while, on the other hand, a cardiologist would require different ones.
- Varied Privileges:
Surgical specialists require delineation of privileges at hospitals, which is a step that primary care doctors in the same practice do not have to go through.
- Ancillary Services:
Practices that provide physical therapy, lab, or diagnostic imaging services have to separately credential these services along with the supervising provider’s credentialing.
- Location-Specific Rules:
If your practice operates at more than one location, each location may have to be linked separately to the provider’s profile with each payer, which results in increased administrative work.
Therefore, this complexity requires a standardized, organized approach.
- Telehealth Credentialing Complexity:
Telehealth credentialing has become one of the biggest challenges for multi-specialty practices in 2025. Payers apply different rules for “Originating Site” (patient location) versus “Distant Site” (provider location) credentialing. Providers may be fully credentialed in one state yet denied reimbursement if telehealth enrollment requirements are not correctly aligned across state lines and payer policies, making telehealth a major source of claim denials.
4. The Complete Medical Credentialing Checklist for 2025
The average turnaround time is 90 to 150 days. Use this checklist to stay on track.
Phase 1: Document Collection & Preparation (1-2 Weeks)
- Identity: Government ID, SSN, NPI, updated CV (MM/YYYY format required).
- Licensure: State licenses, DEA, CDS, Board Certifications.
- History: Malpractice claims history (past 10 years), peer references (3), work history (past 5-10 years with zero unexplained gaps)
- Identifiers: CAQH ProView login, PTANs (Medicare/Medicaid).
Phase 2: Verification & Submission (Weeks 4-8)
This is the “Primary Source Verification” (PSV) stage. You must verify credentials directly with the issuing body, not just trust the paper document.
- CAQH Attestation: Ensure the profile is attested. Most commercial payers pull directly from here.
- Submit Applications: PECOS (Medicare), State Medicaid portals, and individual commercial payers.
- Verify Sources: Contact Medical Boards, Medical Schools, and the NPDB (National Practitioner Data Bank).
Phase 3: Committee Review (Weeks 8-14)
- Payer Committees: Review usually happens monthly.
- Hospital Committees: Often meet monthly to grant privileges.
Phase 4: Maintenance & Compliance (Ongoing)
- Directory Compliance (No Surprises Act): You must verify and update your provider directory information every 90 days. Failure to do so can result in penalties or the provider being suppressed in patient searches.
- Monthly Monitoring: It is no longer sufficient to check licenses every 2 years. Best practice for 2025 is monthly monitoring of OIG exclusions and license sanctions.

5. Overcoming Common Credentialing Challenges
Even with a perfect checklist, pitfalls can emerge. Here are the most common challenges and how to solve them.
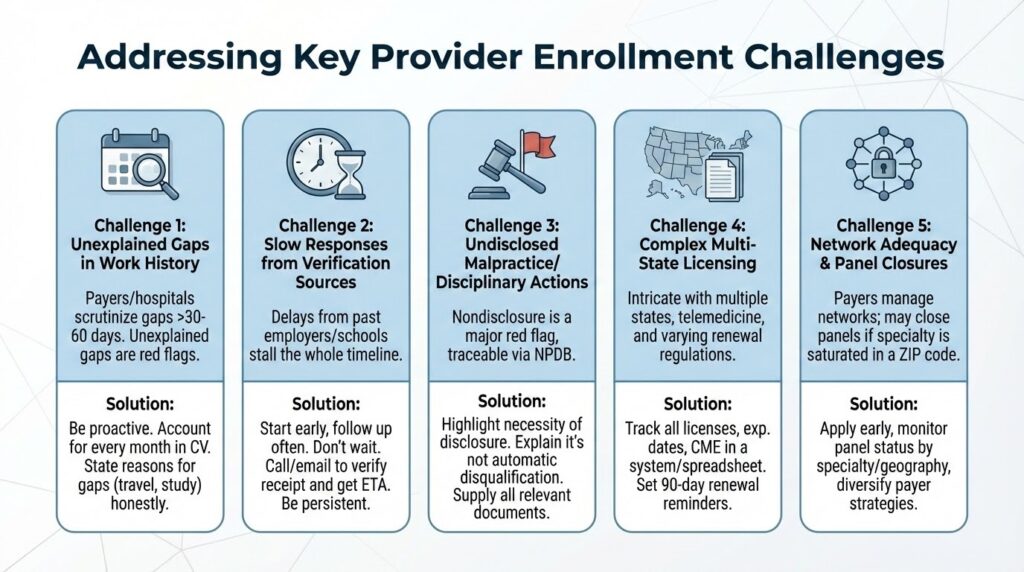
Challenge 1: Unexplained Gaps in Work History
Payers and hospitals are required to scrutinize any gaps in employment or training that exceed 30-60 days. An unexplained gap is a major red flag.
Solution: Be proactive. When compiling the provider’s CV, ensure every month is accounted for. If there was a gap for travel, family leave, or study, simply state it. Honesty and transparency prevent suspicion and follow-up questions.
Challenge 2: Slow Responses from Verification Sources
It doesn’t matter if your team has done everything correctly already because if a past employer or medical school takes its time in responding to verification requests, the whole timeline gets stalled.
Solution: Start follow-ups early and keep doing them often. Don’t let several weeks pass by without checking on a request. After a couple of days, ring up and send an email to the source to verify they got the request and inquire about the estimated time for their response. Keep on doing persistent and professional follow-up which is very important.
Challenge 3: Undisclosed Malpractice or Disciplinary Actions
Some providers may be reluctant to reveal a previous malpractice suit, especially if it was dismissed. Nevertheless, these occurrences can be traced through a National Practitioner Data Bank (NPDB) query and nondisclosure is considered a major red flag.
Solution: Highlight the necessity of thorough disclosure. Assure the providers that a claim will not automatically disqualify them but not disclosing it will. Supply all documents relevant to the situation, which includes the type of claim and the final ruling, in order to clear the misunderstanding transparently.
Challenge 4: Complex Multi-State Licensing
Licensing can get quite intricate when multiple states are involved, especially in the case of telemedicine or border state practices. During the process, adding the different renewal requirements and regulations for each state obfuscates the situation even more.
Solution: Keep track of every license, its expiration date, and its particular CME requirements using a credentialing management system or a comprehensive spreadsheet. At least 90 days ahead, set renewal reminders.
Challenge 5: Network Adequacy & Panel Closures
In 2025, payer enrollment decisions are no longer based solely on provider qualifications. Many payers are actively managing network adequacy, and if a network already has enough providers of a certain specialty within a ZIP code, the payer may close the panel.
Solution: Apply early, monitor payer panel status by specialty and geography, and diversify payer strategies to avoid revenue disruption caused by closed networks.
7. Using Technology to Simplify Credentialing
It’s 2025, there’s no reason to handle credentialing the old-fashioned way. Automated credentialing software can:
- Track provider status in real-time
- Automatically update provider data
- Send alerts when documentation is about to expire
- Generate reports for easy monitoring
The Dastify Solutions Difference: Precision That Drives Profitability
Credentialing delays directly impact your bottom line. At Dastify Solutions, we specialize in accelerating the provider enrollment and credentialing process, ensuring your providers can start generating revenue without unnecessary hold-ups. Our clients experience up to a 40% reduction in Accounts Receivable (AR) and a 95%+ first-pass clean claims rate because our meticulous process eliminates the errors that lead to denials.

To Sum it Up
For a multi-specialty practice, mastering provider enrollment and credentialing process is not only a necessity but also a step towards financial success. By adopting a detailed medical credentialing checklist, understanding the unique payer credentialing steps for each specialty, and by tackling the common challenges proactively, you can cut down the onboarding delays considerably
Implementing a structured system, whether in-house or with a trusted partner, ensures your providers can focus on patient care while your practice thrives financially. Organization, transparency, and persistence are the keys to turning a complex administrative task into a smooth and efficient workflow.