Key Takeaways
- MIPS – or Merit-based Incentive Payments System – is essentially a CMS program that was kicked off in 2017 under MACRA. It ties Medicare Part B payments to how well healthcare providers are doing when it comes to quality, cost and how well they use health IT rather than purely on how many services they do. Your MIPS score out of 100 will decide whether you get a payment bump or a hit on your future Medicare reimbursements.
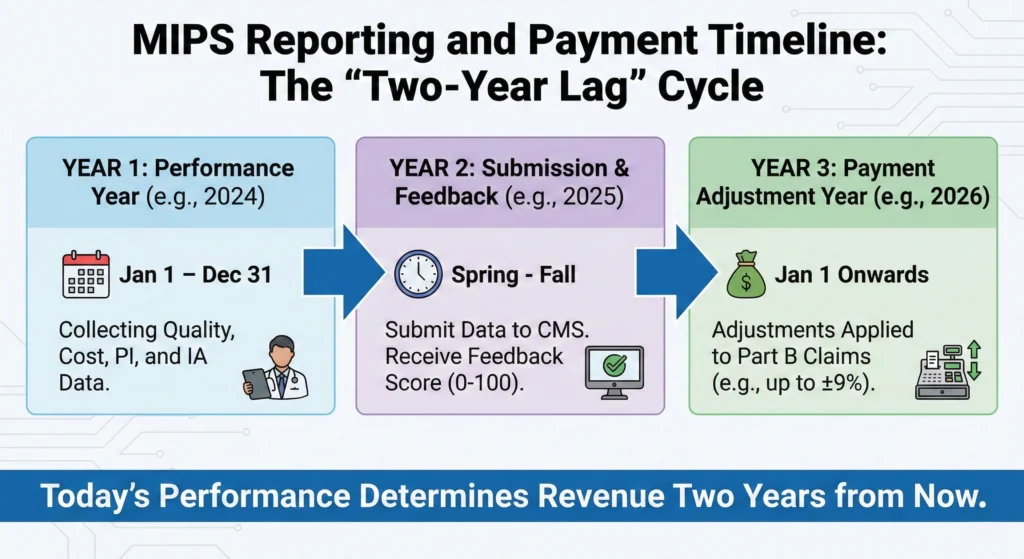
- Payment adjustments can go up to plus or minus 9% of your Medicare Part B allowed charges – and this happens 2 years after your performance year. So, for example, how you do in 2024 will affect how much you get paid in 2026 – which makes today’s reporting decisions really important for your long-term revenue.
- MIPS scoring is based on four main performance categories – Quality (30%), Cost (30%), Promoting Interoperability (25%) and Improvement Activities (15%). And these weights can change from year to year depending on what the CMS says and individual exemptions.
- Most healthcare professionals eligible for MIPS can report as individuals, groups, subgroups or through APM Entities and MIPS Value Pathways. And if you’ve got a low volume of patients, you might be exempt from having to participate, but lots of people still choose to opt in.
- From our perspective at Dastify Solutions, getting a good MIPS score is both a must for compliance and a major revenue cycle opportunity – and having good billing, coding and reporting workflows can make MIPS much less of a headache and more of a competitive advantage.
What Is MIPS in the Healthcare Industry?
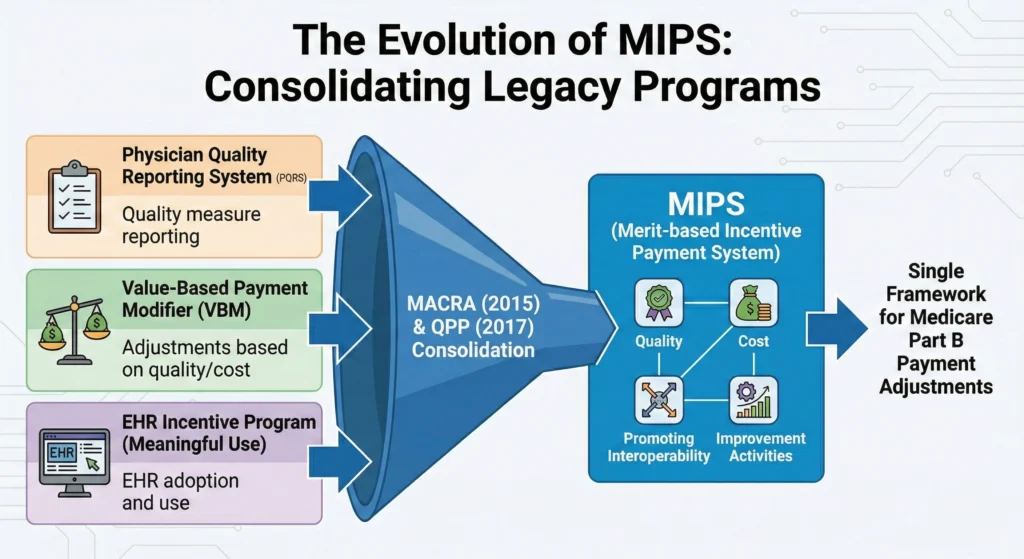
MIPS stands for Merit-based Incentive Payments System – the brainchild of the Medicare Access and CHIP Reauthorization Act of 2015 and launched by the CMS on January 1, 2017 as part of the Quality Payment Program (QPP). And what it has done is fundamentally change the way clinicians get paid for Medicare Part B services.
MIPS is for clinicians and groups who bill Medicare Part B and essentially brings together three legacy reporting programs under one roof.
Legacy Program
What it covered
- Physician Quality Reporting System (PQRS): reporting quality measures
- Value Based Payment Modifier (VBM) : adjusting payments based on quality & cost
- Medicare Electronic Health Record Incentive Program (Meaningful Use) adopting and using electronic health records
Each healthcare provider or group gets a MIPS score out of 100 based on their performance in four MIPS categories – and that score then determines whether you get a payment bump or a hit on your Medicare Part B claims.
The good news is the program is budget-neutral at the national level – so any penalties taken from low performers get reinvested into bonuses for the high performers.
For healthcare providers, MIPS is now an integral part of your value based care strategy – and it needs to be aligned with your billing, clinical documentation and coding systems to maximize both compliance and reimbursement.
MIPS 2025 vs. MIPS 2026 – What’s Changed?
What stays the same
- The way the low volume threshold is calculated – using 2 12-month segments of Medicare Part B data
- The four MIPS performance categories – although the weights can change
- The rules for who gets a pass due to a low volume of patients
Low Volume Threshold Criteria (check with CMS for the current figures)
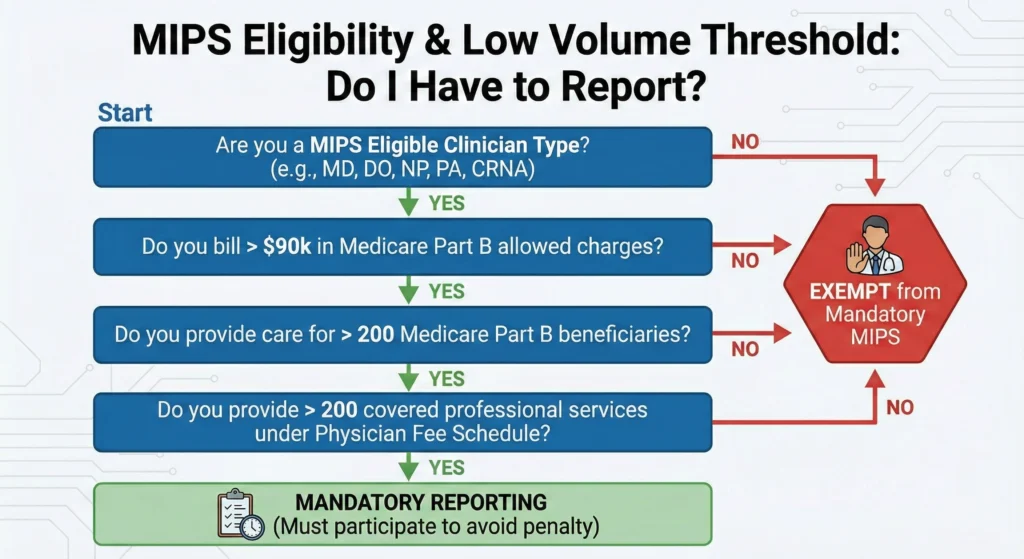
If you’re one of the clinicians who are exempt from having to do MIPS because of the low volume threshold, that’s probably because you’re billing less than $90,000 in allowed Part B charges and seeing fewer than 200 Part B patients or delivering fewer than 200 services during the determination period.
What Changes Every Year
- The quality measures that are available for reporting
- The Improvement Activities options and how they get documented
- The Promoting Interoperability performance category tech specs
- The benchmarks used to calculate performance category score results
- The Cost measures and episode definitions
At Dastify Solutions, we help our clients stay on top of all the rule changes and interpret the annual final rule so that they can adjust their workflows and documentation systems without disrupting their day-to-day operations. This proactive approach means that you’ll avoid last-minute scrambles that can lead to reporting errors and missed opportunities.
Who Has to Report MIPS?
Whether or not you have to do MIPS depends on a few key things: what type of clinician you are, whether you’re exempt due to a low volume of patients and whether you’re taking part in certain Advanced Alternative Payment Model arrangements or MIPS APMs.
The types of clinicians that CMS says are usually included in MIPS:
- Doctors
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Certified registered nurse anesthetists
- And some other types of healthcare professionals – like physical therapists and occupational therapists
And we should warn you that CMS can add new clinician categories to the eligible list through rulemaking – so this list may change over time.
What’s the Low Volume Threshold all about: Clinicians working with Medicare Part B who fall short on their billing and patient counts are usually cut out from mandatory reporting. But some will take the voluntary route – opting in if they meet some of the criteria – while others will report just to get a handle on their performance or maybe even snag some positive adjustments.
APM Participation and Exemptions
Clinicians participating in certain Advanced Alternative Payment Models who make the grade for “Qualifying APM Participant” status can sidestep traditional MIPS and instead get incentives through the APM performance pathway. MIPS APM participants do get a MIPS score, but it’s figured out under the APM’s own rules, which usually yield higher results.
Virtually all the bigger Medicare Part B providers have to play MIPS, making it a key part of their reimbursement strategy and a way to stay compliant.
Individual vs. Group and Other Participation Options
MIPS gives you a lot of flexibility in how you report, which can really affect your scores and payments. Deciding on which way to go is a strategic call that can impact how much effort you have to put in and how much you’ll get back.
Individual Reporting
Your performance is tied to your own NPI and TIN combination. The data and scores are specific to your own encounters and docs. This gives you the most control, but it also means you’ll need to deal with things like data completeness and measure selection on your own.
Group Reporting
If you’re working together with other clinicians under one TIN, you’ll get your scores and measures on a group level. The group’s performance will decide the payment adjustments for everyone involved. We’ve seen that groups and APM Entities often do better than individuals – back in 2018, the data showed this to be the case.
Virtual Group Option
Solo operators or smaller practices can team up with other TINs to report together, without actually merging. This way, you can get some of the benefits of group reporting without actually becoming one.
Emerging Options
| Option | Description | Best For |
|---|---|---|
| MIPS Value Pathways (MVPs) | Specialty-specific measure sets | Specialty practices |
| Subgroup Reporting | Subsets within a group report around specialty or condition themes | Multispecialty groups |
| APM Entity Reporting | Performance is assessed through APM-specific rules | ACO and bundled payment participants |
Pros and Cons
Groups may be able to smooth out individual underperformance, but they do need a good system for capturing data across their whole team. Meanwhile, individuals get to keep control, but they’re usually on their own when it comes to documentation and reporting. Subgroups give you a way to focus on specialty relevance, while still being part of the bigger team.
Dastify Solutions helps practices pick the right reporting model based on their size, specialty mix, and data capabilities – we figure out a way to get the most out of MIPS while keeping administrative headaches to a minimum.
MIPS Performance Categories
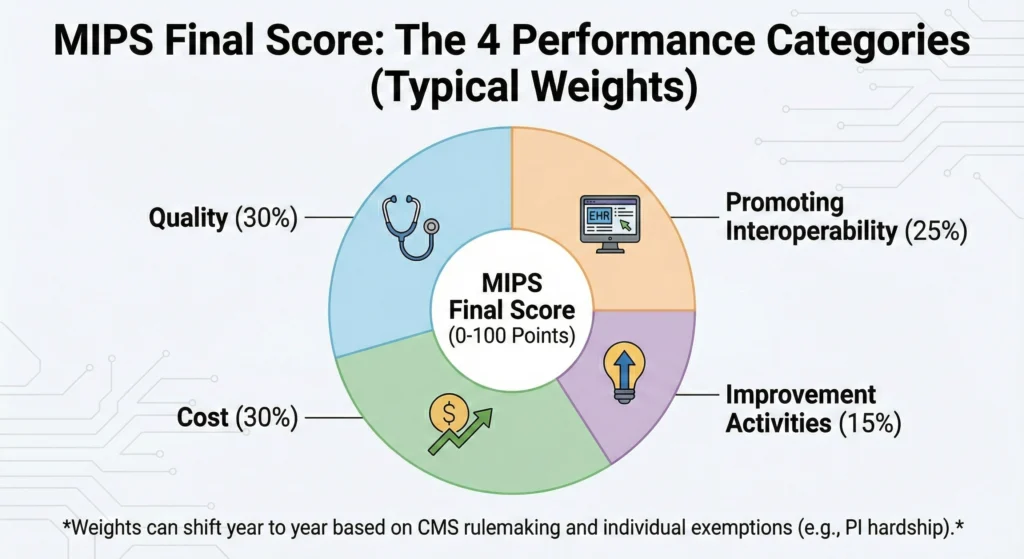
MIPS scores are based on four categories: Quality, Cost, Promoting Interoperability (PI), and Improvement Activities (IA). Each category gets a weight that adds up to 100% of the final MIPS score.
Typical Weights
| Category | Weight | Data Source |
|---|---|---|
| Quality Performance Category | 30% | EHR, registry, claims, QCDR |
| Cost Performance Category | 30% | Medicare claims (CMS-calculated) |
| Promoting Interoperability Category | 25% | Certified EHR data |
| Improvement Activities Performance Category | 15% | Attestation |
CMS can change the weights from year to year, and some exemptions (like PI hardship or lack of cost data) can shift the remaining categories around. To get the best scores across all categories, you’ll need accurate documentation plus clean billing data.
Quality Category
The quality category usually counts for about 30% of the final MIPS score (maybe more, depending on PI or Cost). It’s basically a replacement for the old PQRS system.
Reporting Requirements
- Report at least six quality measures for a full performance period
- Include at least one outcome or high-priority measure
- Pick from a list of about 200-300 CMS-approved measures, many of which are specialty-specific
Common Data Sources
- eCQMs from certified electronic health records
- Clinical quality measures via qualified registries or qualified clinical data registry submissions
- Medicare Part B claims measures
- CAHPS for MIPS survey for patient experience and patient engagement metrics
Your performance is compared to national benchmarks, with each measure translating to points. Small practices get a break on scoring by getting bonus points for limited case volumes, or special considerations.
Dastify Solutions’ coding, encounter capture, and denial management keep you ahead of the game by getting services both billed and documented right.
Promoting Interoperability (PI)
The promoting interoperability performance category usually accounts for about 25% of the overall MIPS score, and it focuses on getting certified electronic health record technology (CEHRT) doing its job to share health information securely and get patients more engaged.
Core Requirements
- Use 2015 Edition (or successor) CEHRT for at least 90 continuous days within the performance year
- Mandatory measures include e-prescribing, providing patients electronic access, health information exchange, and public health reporting Both of the main requirements and performance-based scoring determine final category points
Hardship Exceptions Are Available For
- Small practices with fifteen or fewer clinicians
- Practices with limited internet access
- Certain clinicians working in a hospital setting
- Practices facing extreme circumstances
Having a strong EHR integration with scheduling, documentation and billing systems means that PI workflows just become another part of normal clinical practice rather than extra administrative tasks than the rest of the practice.
Dastify Solutions prioritizes a seamless integration with EHR so that the billing and clinical data needed for PI reporting all align up and are easily verifiable – which in turn supports both patient outcomes tracking and making sure your reporting is accurate.
Improvement Activities (IA)
The improvement activities category usually makes up 15% of the mips score and rewards practices for doing structured work that improves clinical practice through better care co-ordination, patient safety, access and population health management
How Activities Are Structured
- CMS offers a selection of medium-weight and high-weight activities in a catalogue
- Examples include keeping longer hours, doing care management for complex patients, expanding telehealth and patient-specific education
- Clinicians then need to attesting to having completed a certain number of activities over at least a 3 month period, weighted to reflect their difficulty
Special Considerations
- Small, rural or HPSA practices might need fewer activities to reach the full credit
- Documentation requirements are more flexible for qualifying small practices
- Evidence that the initiative was actually implemented needs to be kept in case of any audit
A lot of IA options overlap with initiatives that well-run practices are already undertaking – chronic care management, referral tracking and enhanced communication protocols. The main thing is to formalise, document and make sure these efforts align with CMS activities so as to boost clinical practice quality scores
Dastify Solutions can help map out existing initiatives to specific IA’s and make sure the supporting documentation (like policies and reports) is kept safe for compliance.
Cost Category
The cost performance category usually accounts for around 30% of the mips score and is calculated entirely by CMS using Medicare claims data – no direct data submission from clinicians is required here.
What Cost Measures Are Evaluated
- Total spending for all Medicare patients attributed to the practice
- Spending for specific episodes of care (like total cost of care or a condition specific episodes)
- All measures are risk-adjusted to take into account patient complexity
Why Accurate Coding Is So Important:
Even though clinicians don’t submit cost data themselves, their patient selection, care co-ordination, coding and referral patterns do all influence the costs and benchmarks attributed to the practice. CMS uses 25 cost measures which are automatically calculated from claims data.
Inaccurate coding or under-documentation can mess up the risk adjustment, making patients seem less sick than they actually are and making the practice look worse comparatively – and that can lead to a sneaky penalty that a lot of practices miss until they look over their performance feedback.
Dastify Solutions’ focus on accurate ICD-10 and CPT/HCPCS coding, plus proactive denial management and analytics, helps capture the accurate risks and costs in MIPS scoring.
How The MIPS Final Score (CPS) and Payment Adjustments Work
The final MIPS score – or composite performance score – is a summary of the practice’s progress that’s used by CMS to decide on MIPS payment adjustments two years after the performance period finishes.
How the Score Is Calculated
- Each category’s raw performance is turned into a point value (capped at the category maximum)
- Category points are multiplied by their respective weights
- Weighted scores are added together to produce the final performance score
- The final score is then compared against the annual performance threshold
Example Calculation
| Category | Points Earned | Weight | Weighted Contribution |
|---|---|---|---|
| Quality | 80 | 30% | 24.0 |
| Cost | 70 | 30% | 21.0 |
| PI | 90 | 25% | 22.5 |
| IA | 40 | 15% | 6.0 |
| Total | 73.5 | ||
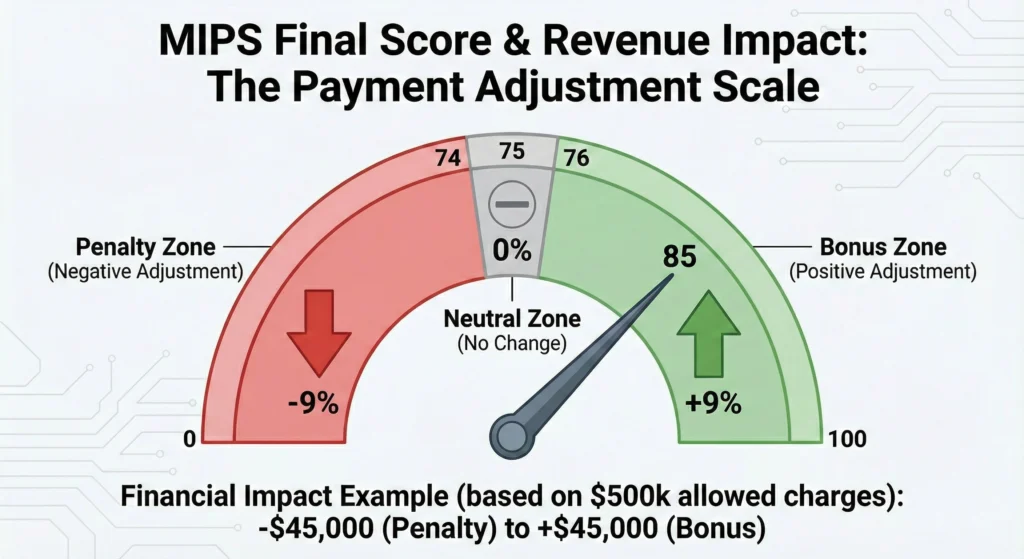
Performance Threshold and Adjustments
CMS sets an annual performance threshold – in the last few years this has been around 75 points. Clinicians need to meet or exceed this threshold to avoid penalties:
- Scores below threshold – Negative payment adjustment
- Scores at threshold – Neutral adjustment (no change)
- Scores above threshold – Positive payment adjustment
- Very high scores – Potential additional bonus (where applicable)
Maximum adjustments have been increasing over time, and now can reach ±9% of Medicare Part B allowed charges associated with MIPS-eligible services, subject to budget neutrality.
Even a few points can make a difference to the bottom line for high-volume practices. Dastify Solutions uses analytics to find quick-win opportunities – targeted quality measures, PI optimization, documentation fixes – to push scores above the threshold and maximize reimbursement.
Minimum Score to Avoid Penalties
CMS publishes a specific performance threshold each year that clinicians need to reach to avoid a negative payment adjustment on future Medicare Part B reimbursements.
Recent Threshold History
The threshold has mostly been around 75 points in recent program years, but the exact threshold is defined annually in CMS rulemaking and can shift based on program maturity and policy goals.
Score Outcomes
| Score Range | Payment Impact |
|---|---|
| Below threshold | Negative adjustment with progressive penalties – up to 9% less revenue |
| Performance Level | Payment Impact |
|---|---|
| On the Brink of Trouble | Neutral adjustment |
| Just Over the Threshold | Positive adjustment starting to add up |
| Real Standouts | Additional bonus where it’s available |
Critical Warning
Not reporting data when you should be is a recipe for disaster – an automatic max negative penalty is waiting for you. Even half-hearted, strategic reporting beats non-participation for avoiding financial meltdown.
The Real Bottom Line
For a practice of average size with $500,000 in annual Medicare Part B allowed charges, a 9% hit takes away $45,000 in revenue. On the other hand, a 9% boost brings in $45,000. We’re talking a $90,000 swing between best and worst case – that’s a clear call to make MIPS a priority.
Lowering the Barrier to Entry for Small Practices
CMS defines small practices as those with 1-15 eligible clinicians under a single TIN. These organizations get a break on administration.
Rulebreakers and Exceptions
- Bonus points automatically added in certain categories (for example Quality)
- Lower reqs for improvement activities for full credit
- Easier attestation for improvement activities
Where to Get Help
- Hardship exceptions for interoperability
- Targeted technical support
- Pool resources by joining a virtual group
- Participate via a registry or qualified clinical data registry to make things easier
Some Practices Just Need More Support
Small practices are hit hard by manual reporting and lack of compliance resources. Reporting reg reqs can swamp teams already doing their best to keep up with patient care.
Partners like Dastify Solutions can take a weight off your shoulders by handling RCM and MIPS workflow. Still, small practices face real risk of penalties and so treating MIPS as a top financial and compliance priority is essential.
MIPS Value Pathways (MVPs) – The Future of Reporting
CMS is shifting MIPS towards more streamlined, specialty specific reporting options: MIPS value pathways and MIPS APMs.
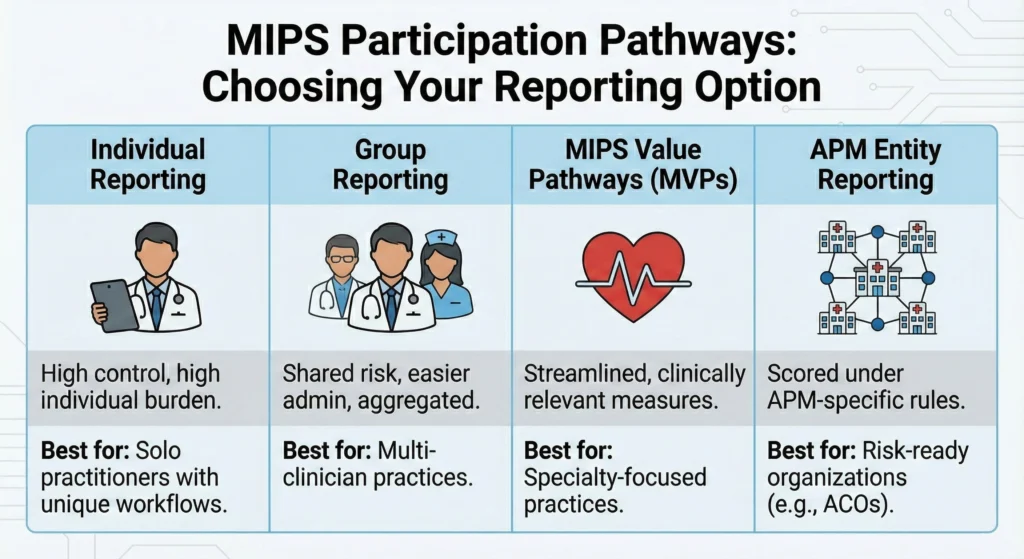
What are MVPs?
MVPs are measure sets tailored to individual specialties or groups of conditions (cardiology, diabetes care etc). They link Quality, Cost and other measures around a single clinical theme, making scores more meaningful.
Eligibility
- Individual clinicians
- Groups
- Subgroups
- Some Alternative Payment Model entities
What are MIPS APMs?
These are models like ACOs or bundled payments, where participants are still scored but with APM rules. Published analysis shows APM MIPS participants often get higher median scores than traditional MIPS participants.
Choosing Your Path
| Pathway | Best For | Key Advantage |
|---|---|---|
| Traditional MIPS | General practices, diverse specialties | Most flexible |
| MVPs | Discipline-specific practices | Clinically relevant, easier |
| MIPS APMs | Risk-ready organizations | Higher potential scores |
Dastify Solutions can help determine whether MVPs, traditional MIPS, or APM participation will work best for your practice.
What Dastify Solutions Offers
At Dastify Solutions, we see MIPS as part of the big picture – a partner with your billing, coding, and documentation excellence. We know that MIPS reporting needs more than just a checkbox – it needs a way to grow and protect your Medicare revenue.
Better Billing and Coding Support
Our ICD-10, CPT, HCPCS coding services capture all clinically relevant services, supporting Quality and Cost scoring. Your revenue stream benefits from accurate coding, improved cost attribution and risk adjustment accuracy.
Cloud Based Tools and EHR Integration
Our cloud-based tool, EHR/EMR integration and registry solutions ensure clean, structured quality data gets to where it needs to go, eliminating the manual data reconciliation that causes so many reporting errors.
Expertise that Matters
Our team has deep experience and knowledge across specialties, including home health, cardiology, ortho, and behavioral health. This lets us align your billing with the right measure sets or MVPs, maximizing scores while keeping things clinically relevant.
Supporting your Business:
- Denial and AR management to keep cash flow from drying up
- Payer and enrollment support to prevent billing gaps
- Compliance audits to ensure you’re following the rules
- Quick-win analysis to improve your scores
FAQs
How far back do MIPS performance periods affect my Medicare payments?
MIPS performance years (2024 being a prime example – January 1st to December 31st) tend to affect payment adjustments two years down the line (with 2026 being the year that matters for claims). So if you’re thinking about what measures to choose, how to document stuff and what to report on today, you’re laying the groundwork for what you’ll be getting paid for several years from now. Being a few steps ahead is what matters when it comes to getting the best reimbursement deals long term.
Does MIPS apply to Medicaid or commercial payers, or only Medicare Part B?
MIPS specifically only applies to Medicare Part B via the Medicare and Medicaid services. But loads of commercial and Medicaid plans have their own take on value-based care and may use similar metrics in their contracts. Working on making your documentation and reporting system MIPS-friendly will likely serve you well with other payers too.
What happens if my practice switches EHRs or billing systems mid-year?
Switching over mid-year can cause some serious issues with measure calculations and making sure all your data is there. To avoid any problems try maintaining data exports across both systems for a bit, make sure the new system you choose is CEHRT certified so you meet the requirements and don’t get left behind, and get in touch with a pro like Dastify Solutions to help you iron out any discrepancies come end of year. Planning ahead around the MIPS performance calendar will make things a lot more manageable.
Can I still get a positive MIPS adjustment if I only report a subset of measures?
The thing to keep in mind is that CMS has some pretty strict requirements around data completeness and case counts. Reporting on just a few measures might still get you some points, but if you don’t meet the minimum requirements you might miss out on some or all of those points, which isn’t ideal. The trick is finding the right balance – pick the measures that really matter, but still make sure you’re meeting all the necessary requirements so you don’t get left with nothing.
How often does CMS audit MIPS data, and what kind of documentation should I be keeping?
CMS (and their contractors) like to give MIPS submissions a good once-over – they do random and targeted audits. To be on the safe side it’s a good idea to keep all the supporting documentation for at least 6 years after the performance year, that includes EHR logs, reports, policies, screenshots, billing data and anything that proves you were on the right track. This will give you some peace of mind and help you avoid any potential audit penalties.