Key Takeaways
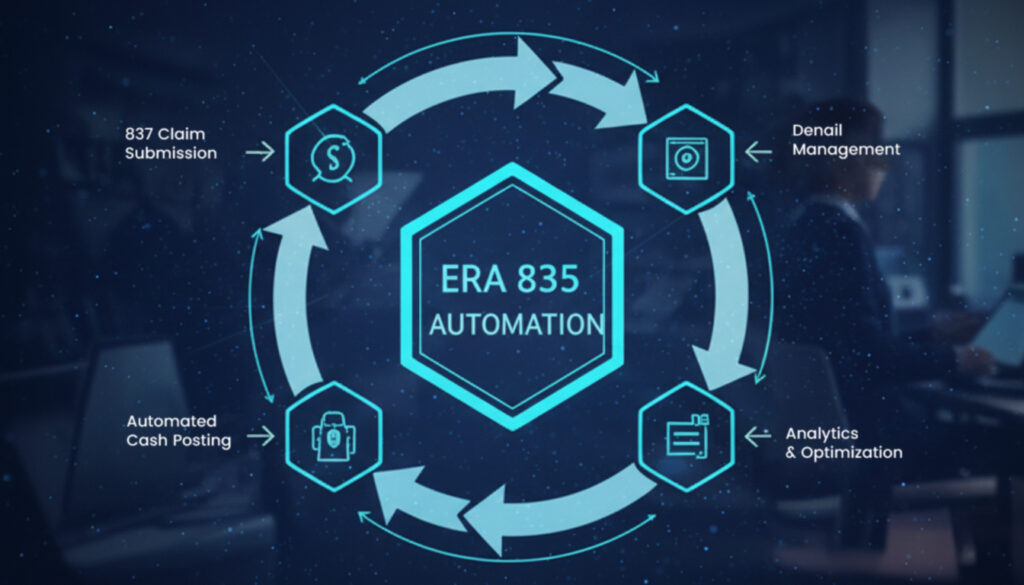
- ERA 835 is the HIPAA EDI 835 electronic remittance advice transaction that payers use to give healthcare providers the lowdown on claim payments, denials, and adjustments.
- Getting 835 processing right is absolutely crucial for clean cash posting, denial management, and making sure your 837 claim submissions line up with payers like Medicare, Medicaid, and commercial payers.
- Mistakes or misconfigurations in 835 workflows – including file format issues, getting the mapping wrong, or problems when posting to the bank – can seriously delay getting paid and make manual work for your billing team way more than it needs to be.
- The healthcare industry is throwing an estimated $1.5 trillion a year at repetitive administrative tasks – which is why 835 automation should be a top priority for cost reduction.
- Dastify Solutions comes to the rescue with AI-driven tools and services to automate 835 ingestion, posting, and reconciliation, and is helping healthcare organizations in all 50 states to cut down on days in A/R and write-offs.
What is The Deal With ERA 835 in Medical Billing?
So here’s the deal with the ERA 835, also known as EDI 835 – it’s the electronic remittance advice transaction that payers use to send out payment and adjudication info to healthcare providers. When an insurance company processes a claim and makes a payment decision, the 835 file is how they let the provider know exactly what happened – what got paid, what got denied, and why.
Think of the 835 file as the electronic equivalent of a paper Explanation of Benefits (EOB) document, but instead of being a snail-mail paper trail, it’s in a standardized electronic format under HIPAA (ASC X12N 005010X221A1) which makes it machine-readable and perfect for automated processing without needing to be manually reviewed.
ERA 835 files come in from virtually every payer in the US healthcare system, including:
- Medicare Administrative Contractors (MACs)
- State Medicaid programs
- Commercial insurance carriers
- Workers’ comp payers
These remittance advice files usually come in along with electronic funds transfer deposits, checks, or virtual card payments – and the 835 tells you not just that money arrived, but exactly where to put it across your claims and patient accounts.
Here’s how the 835 is supposed to fit into your revenue cycle workflow:
- You submit an 837 claim (professional or institutional) to the payer
- The payer goes through claim adjudication, checking the claim against benefits, contracts, and medical policies
- The payer spits out an 835 ERA with their payment decisions (paid, denied, adjusted)
- The 835 comes back to you, usually through a clearinghouse or a direct connection
- Your billing team posts payments, denials, and patient responsibility amounts
Dastify Solutions uses these standardized 835 files as the basis for automated payment posting, denial capture, and analytics for clients in all 50 US states – by treating the 835 as data that can be easily processed, rather than some document that needs to be manually read.

How ERA 835 Relates to 837 Claims and EFT Payments
Getting a handle on the relationship between 837 claims, 835 remittances, and electronic funds transfer payments is essential for anyone in charge of healthcare billing.
Here’s how the cycle works: your organization submits an 837 transaction (institutional 837I for hospital claims or professional 837P for physician services) to a payer – and after the payer has done their adjudication, they send out two things at the same time: an EFT deposit into your bank account, and an 835 ERA file that says exactly how each claim line got paid, adjusted, or denied.
Some important things to keep in mind
The payer lets the provider know what they decided – what got paid, what got denied, and why.
You’ll often get one 835 that references multiple claims from previous 837 submissions – your Monday morning deposit might include a single 835 that covers 200 individual claims. And sometimes one original claim might show up in multiple 835 files – e.g. when a payer sends a partial payment followed by a subsequent adjustment or recoupment.
The EFT deposits via ACH or other electronic payment rails, and the 835’s BPR and TRN segments tell you exactly how to match the bank transaction to the remittance file – so that you can reconcile your deposits with the claim information.
Timeframes vary by payer – here’s a rough idea of what you’re looking at:
- Medicare: 14-30 days from claim submission to payment
- Medicaid: varies by state, usually 30-45 days
- Commercial payers: 15-45 days depending on contract terms
Delays at any point in this cycle are going to impact your cash flow – when an 835 arrives late or doesn’t line up with your expected payments, your revenue cycle team is going to have to scramble to get things sorted.
Core Structure and Segments of an 835 ERA File835 Files Explained: Understanding the ASC X12 835 Standard
There are 835 files that follow the ASC X12 835 standard, helping to organize all the important stuff like who owes who, who’s getting paid, what the claims are, and what services are being rendered into a neat little hierarchical structure of segments and loops. Grasping this structure is key to getting paid on the money – and figuring out what’s gone wrong when things don’t go right.
The ASC X12 835 has a layered way of organizing this data:
Breaking Down the File Structure
The file uses a somewhat clunky but effective “envelope” approach:
- ISA/IEA: The main envelope that wraps everything together. This is where you’ll find the clearinghouse or payer sending you the money.
- GS/GE: These are the functional group headers. They group related transactions together and make it easier to find what you need.
- ST/SE: These are the transaction set boundaries, which help mark the start and end of each 835 remittance.
- BPR: The payment order details. This is where you’ll find the payment amount, payment method and date.
- TRN: The trace number. This is a unique number that your bank and payer can use to track payments and help you figure out what to do with them.
- N1: This is how you identify the payer and payee – the insurance company and the provider getting the cash.
- CLP: This is where the claim payment information lives – including per-claim totals, status and references.
- SVC: This is the service payment detail. Each line-item here breaks down the payment by individual procedure.
- CAS: The claims adjustments – including the reason codes and adjustment amounts for each claim.
Loops Organize the Data Hierarchically
Here’s how the loops all fit together:
- Loop 1000A (Payer): This is where you find the insurance company that’s sending the money
- Loop 1000B (Payee): This is where you find the provider getting the cash
- Loop 2000 (Header): Transaction-level payment information
- Loop 2100 (Claim Payment): This is where you find the individual claim level details
- Loop 2110 (Service Payment): This is where you find the line-item detail for each service
If you can get your head around these loops, you’ll be able to figure out which EHR or practice management fields get populated and what reports your finance team can generate. But it’s a complex beast. Dastify Solutions maps the payer-specific Companion Guide rules to a unified internal schema, so your team doesn’t have to manage all the complexity of different 835 variations from each payer.

BPR and TRN: The Keys to Unlocking the ERA to Actual Funds
The BPR segment, or Beginning Segment for Payment Order/Remittance Advice, carries a lot of critical payment information:
- Payment type (ACH, check, etc)
- Total payment amount for the transaction
- Payment date
- Bank account and routing information
If this segment says $47,832.16 was deposited on June 15th, your bank statement should show the same on that date. The TRN segment, or Trace Number, is a unique identifier that banks and payers use to track payments. This number becomes the key for matching the ERA to the actual deposit and creating auditable posting batches.
Some common problems that create headaches for billing teams include:
- Missing TRN values that make deposit matching impossible
- Duplicate TRNs that cause confusion about which 835 is which
- Misaligned BPR amounts where the payment total doesn’t match posted claims
- Multiple 835 files tied to a single EFT deposit
CLP, SVC, and CAS: Claim and Line-Level Payment Detail
The CLP segment reports all sorts of useful information at the claim level:
- Claim submitter identifier (patient control number)
- Claim status code (paid, denied, processed as primary, etc.)
- Total charge amount
- Total payment amount
- Patient responsibility amount
- Payer’s claim number
The SVC segment breaks down payment by individual procedure:
- CPT or HCPCS code
- Billed amount
- Paid amount
- Allowed amount
- Units of service
- Revenue codes (for institutional claims)
And the CAS segment is where denial management lives, with each CAS segment including:
- Adjustment Group Code: CO (Contractual Obligation), PR (Patient Responsibility), OA (Other Adjustment), PI (Payer Initiated Reduction)
- Adjustment Reason Code: Specific codes like CO-45 (charge exceeds fee schedule), PR-1 (deductible), CO-97 (bundling)
- Adjustment Amount: Dollar value of the adjustment. Dastify Solutions uses CLP/SVC/CAS figures to drive automated posting rules, categorize denials by root cause and flag up contract variances for RCM bosses. When you can get on top of every adjustment reason code, you begin to notice patterns – often 30% of your cardiology denials are down to CO-97 bundling issues that can be sorted out with some coding education.
Operational Headaches with ERA 835 Files
Even with the standardization that HIPAA offers, real-world 835 processing is still a right old pain in the neck.
The Industry is Plagued By
- Payers sending 835 files that are either incomplete or in a non-standard format that breaks your parsing routines
- Mismatched identifiers between 835 claim references and the original 837 patient control numbers
- Late remittance files that turn up days after the EFT deposit
- Inconsistent use of CAS denial codes across different payers
- Missing SVC segments that stop you posting line by line
Reconciliation is a Nightmare
- One EFT deposit covering multiple 835 files that you have to manually stick together
- 835 files that reference multiple payment dates or bank deposits
- Adjustments (recoupments, interest, penalties) from PLB’s that don’t tie to specific claims
- Reversals and takebacks appearing weeks after the original payment
Without Proper Automation, You Risk Misposting
- Payments being applied to the wrong patient account due to identifier mismatches
- Wrong location or NPI being credited, which skews departmental reporting
- Incorrect GL account assignments causing month-end reconciliation fouls
- Manual errors from billing staff entering data from paper EOBs

Specialty-specific Complexity is a Real Pain
- Home health organizations under PDGM have to deal with complex PLB adjustments and retrospective rate changes
- Behavioural health providers often have benefit information tied up in authorisation tracking
- Multi-site groups juggle multiple NPIs, Tax IDs and clearinghouses feeding overlapping 835 streams
- Hospital systems are dealing with both 837I and 837P transactions that need different posting logic
These operational headaches are directly affecting cash flow, blowing up your days in A/R and forcing your billing teams to spend hours on reconciliation instead of looking into denials or servicing patients.
Compliance, HIPAA and Audit Considerations
ERA 835 transactions contain sensitive patient information, including names, dates of service, claim details and payment information. Every organization that handles 835 files has to be on top of HIPAA Security and Privacy Rules.
Transmission Security Requirements
- Payers and clearinghouses typically send 835 files via SFTP, HTTPS APIs or VANs
- Encryption in transit is a must for electronic exchange of patient information
- Encryption at rest protects 835 files stored on your system from getting into the wrong hands
Access Control Requirements
- Role-based access controls so only the right people can view and process the 835 data
- Audit trails showing who accessed what data and when
- Secure credential management for clearinghouse and payer connections
Audit Trail Importance
External auditors need to be able to trace from bank deposit to BPR/TRN to CLP/SVC line items and finally to the practice management or hospital billing system ledger. A well-structured 835 processing system will create this audit trail automatically.
Dastify Solutions has got their security controls sorted, including encryption in transit and at rest, role-based access and detailed audit logging to support both HIPAA compliance and audit readiness.
How Dastify Solutions Makes ERA 835 Processing Easier
Dastify Solutions is a B2B SaaS + services revenue cycle management company offering AI-powered 835 processing and end-to-end billing support for healthcare organizations across all specialties and states.
Core Platform Features
The platform pulls in 835 files from multiple payers and clearinghouses through secure connections. Rather than having to manually sort out each payer’s format quirks, the system reads delimiters from ISA headers itself and normalises the data into a unified cloud database.
Automated Posting Engine Features
- Rule-based posting that can handle standard payment scenarios without needing human intervention
- Machine learning-driven logic for complex edge cases and exception handling
- Automatically splitting patient vs payer responsibility based on CAS group codes
- Categorising denials by adjustment reason codes for instant analytics
- Exception worklists for cases needing a human review (e.g. missing patient accounts, unknown denial codes)
Reconciliation Automation
The system matches 835 data to 837 claim records, patient accounts and contracted fee schedules. This enables:
- Automatic detection of underpayments relative to expected reimbursement
- Identifying recurring denial patterns by payer, provider or procedure
- Reconcile deposits against BPR totals using TRN-based matching
- Alerting when EFT amounts don’t match 835 payment totals
Integration Flexibility
Dastify Solutions integrate with common EHR and practice management systems through APIs, SFTP file drops and HL7/JSON bridges. This allows for near real-time posting and reporting without disrupting existing workflows or replacing your existing systems wholesale.

What Benefits for Providers and Billing Teams
Qualitative Improvements
| Metric | Typical Improvement |
| Manual posting time | 50-80% reduction |
| Days in A/R | Significant decrease through faster posting |
| Posting error rate | Near elimination of manual errors |
| First-pass denial resolution | Improved through systematic categorization |
Qualitative Benefits
- Clearer visibility into payer behavior and payment patterns to drive cash flow predictability
- Standardized denial reason reporting across all payer sources to help you identify areas for improvement
- Timely dashboards showing cash, write-offs, reversals, take-backs, and other key metrics
- Better data for contract negotiations with concrete evidence of underpayment
Specialty-Specific Support
Dastify Solutions supports a wide range of specialties including:
- Cardiology and Cardiovascular Surgery
- Orthopedics and Pain Management
- Behavioral Health and Substance Abuse Treatment
- Home Health Agencies under PDGM and OASIS Requirements
- Skilled Nursing and Hospice Facilities
For CFOs and RCM leaders, the benefits translate to tangible business outcomes: predictable cash flow, lower cost to collect, reduced staffing pressure, and improved compliance posture. The platform boosts productivity by automating high-volume, repetitive tasks so your team can focus on exceptions, appeals, and patient experience.
Best Practices for Managing ERA 835 in Your Revenue Cycle
Whether you handle 835 processing internally or partner with a company like Dastify Solutions, these practices will strengthen your revenue cycle operations.
Daily File Management
- Work out a standardized process for retrieving ERA 835 files daily from all payers – don’t leave it to chance.
- Verify file integrity before posting. check ST/SE control numbers, segment counts, and delimiter consistency. Don’t let errors slip through.
- Don’t let files pile up – process payments promptly to minimize aged A/R
Identifier Management
- Develop a clear strategy for mapping payer claim numbers to your patient control numbers
- Make sure every 837 claim includes identifiers that will appear in the corresponding 835
- Keep track of the right account associations so payments post to the correct patient and encounter records
Denial Taxonomy Development
- Build a denial and adjustment taxonomy based on CAS codes
- Group denial codes into logical categories for targeted intervention
- Track co-pay and deductible responsibility separately from true denials
Reconciliation Discipline
- Reconcile BPR payment totals to bank deposits and GL entries daily or weekly. get it right the first time.
- Investigate any discrepancies between expected and actual deposits. no room for error.
- Track missing ERA files. If you receive an EFT but no ERA, follow up immediately.
- Keep an eye on PLB adjustments for unexpected recoupments or provider-level changes.

Partnership Consideration
Partnering with a specialized RCM and automation provider like Dastify Solutions can take the technical heavy lifting of ERA parsing, mapping, and posting out of your hands. This allows your in-house team to focus on.
What They Do Best: Ensuring coding quality, managing payer relationships, and improving patient experience.
Special Considerations by Payer and Setting
Not all ERA files are created equal. different payers and care settings introduce variations that your billing process must accommodate.
Payer-Specific Variations
- MACs publish companion guides that modify core 835 segment usage
- State Medicaid programs have unique rules for adjustment reason codes and benefit information
- Large commercial payers may use proprietary codes that require translation
Institutional vs Professional Differences
| Setting | Claim Type | 835 Patterns |
| Hospital outpatient/inpatient | 837I (UB-04) | Revenue codes in SVC segments, complex PLB adjustments |
| Physician practice | 837P (CMS-1500) | CPT/HCPCS focus, simpler claim structures |
| Ambulatory surgery | Both possible | Varies by facility structure |
Post-Acute Care Complexity
- Home health under PDGM frequently sees retrospective rate changes and requests for anticipated payment (RAP) eliminations
- SNF and hospice billing involves complex PLB adjustments for consolidated billing
- These settings require robust tracking of claim adjustments over extended episode periods
Dastify Solutions encapsulates these payer- and setting-specific rules into configurable templates rather than one-off scripts maintained by internal IT staff. When Medicare updates its companion guide or a commercial payer changes their CAS code usage, the platform adapts without requiring your team to rebuild posting logic.
FAQ – ERA 835 and Electronic Remittance Advice
Is an ERA 835 file the same as an explanation of benefits (EOB)?
Functionally, yes. The ERA 835 is the standardized electronic version of paper EOBs. It includes detailed information about what was billed, what was allowed, what was paid, what the patient owes, and why any portions were denied or adjusted through adjustment reason codes. The crucial difference is that the 835 is machine-readable in electronic data interchange standard format, designed for automated posting, whereas an EOB is formatted for human reading and requires manual data entry.
Do I really need an 835 ERA if my practice is already getting EFT payments?
Yep – EFT payments tell you money has gone into your bank account but don’t say where it should go across claims and service lines. The 835 ERA matches each dollar in the deposit to specific claims, CPT/HCPCS codes and reason for the adjustment. Without it, your staff are stuck manually trying to work out from paper EOBs where the payments and denials go which is slower, more prone to errors and a lot more time consuming for everyone.
How does having era 835 help with denial management?
The 835 ERA includes CAS segments with codes and reasons for adjustments which tell you exactly why a claim was underpaid or rejected. For example, CO-97 means a bundling reduction, while PR-1 shows the patient is responsible for a deductible. By properly catching and sorting these denial codes, you can figure out where the problems are, prioritize appeals to get the money back and fix issues such as checking patient eligibility or maybe even just how you bill something.
Can small practices really benefit from automated 835 processing or is this only for really big hospitals?
Actually small and mid-sized practices often benefit the most because they’ve got limited billing staff. By automating the 835 ERA, you save time on manual data entry and get the cash in faster without having to hire more staff. Dastify Solutions can set it up so it fits your practice, whether it’s a solo practice or a small to medium-sized group or even a really big health system.
What do I need to get the era 835 automated integration going with my existing EHR or practice management system?
Usually it’s about setting up safe ways for 835 files to get from the payers and clearinghouses to your system, and then mapping those files to the way your system does data, and then setting up the rules for how the payments are posted based on how you do things around the office. Dastify Solutions can sort it out via APIs or file exchange or even through your EHR or PM vendor’s integration hub with minimal disruption. The team works directly with your EHR or PM vendor to ensure the formats match and does all the testing before you go live.
Conclusion
Mastering ERA 835 processing is about a lot more than just ticking all the compliance boxes – it’s about having a smooth and profitable revenue cycle. The difference between struggling with manual posting and getting clean, easy cash applications is having the right systems in place and the expertise to go with it.
If your organization is spending too many hours on payment posting, losing track of denials or struggling to sort out deposits, then it’s time to take a hard look at your 835 workflows. Dastify Solutions can provide the AI-powered automation and the medical billing expertise to turn your remittance processing into a competitive advantage instead of a problem.