A prior authorization denial isn’t the end of the road; it’s a call to action. While fewer than 1% of denied claims are appealed, a structured approach under the Affordable Care Act (ACA), can reverse the majority of medical necessity rejections, helping providers protect patient care and secure approvals faster.
If you’re reading this, chances are you’re facing a prior authorization denial right now and you need answers fast. This blog walks you step by step to protect patient care and secure approvals faster.
How To Get Prior Authorization: Critical First Steps
Step 1: Read the Denial Letter & Type Carefully
Review the denial notice to understand why the request was denied. This determines your next steps.
An Adverse Benefit Determination (ABD) may include:
- Denial of a prior authorization request
- Refusal to pay for services already received
- Determination that treatment is not medically necessary
- Classification of care as experimental or investigational
- Out-of-network service denials
- Coverage rescission or termination
The denial notice must include:
- Diagnosis and procedure codes
- Specific denial reason and denial code
- Plan provisions or medical criteria used
- Information on appeal rights (internal and external)
Tip: If any of this information is missing, you can request it from the insurer at no cost.
Step 2: Check Timelines for the Denial Decision
Knowing the timeline helps you decide whether to pursue a standard or expedited appeal.

What if my care is urgent? If your situation is time-sensitive, you may qualify for an expedited prior authorization review. Mark the case as urgent and provide supporting documentation. Some states or insurers allow simultaneous internal and external review to speed approval. Follow up promptly to ensure your request is processed.
Step 3: Verify Eligibility and Authorization Requirements
Before appealing, confirm the patient’s eligibility and that all PA requirements are complete; many denials result from coverage mismatches or missing paperwork.
What to check:
- Confirm the patient’s insurance coverage for the requested service or treatment.
- Make sure the service requires prior authorization and all forms were submitted correctly.
- Verify that patient information (DOB, insurance ID, policy details) matches exactly what the insurer has on file.
- Check for payer-specific rules, like required supporting documentation or referral forms.

Step 4: Communicate With the Insurer and Provider
Early communication can prevent formal appeals.
Do this:
- Contact the insurer to confirm the denial reason
- Ask whether additional documentation could reverse the decision
- Coordinate with your provider to gather:
- Clinical notes
- Letters of medical necessity
- Supporting medical evidence
Step 5: Gather Supporting Documentation
Once you understand the denial reason, collect all evidence proving the service or treatment is medically necessary. The more organized your documentation, the stronger your appeal.
Key documents to gather:
- Clinical notes from the treating physician
- Test results & imaging reports
- Letters of medical necessity
- Referral letters or specialist evaluations
- Previous approvals or authorizations
Peer-to-Peer Review Opportunity
For medical necessity denials, request a P2P review. This allows your physician to speak directly with the insurance company’s Medical Director. A short clinical conversation can often resolve the denial faster than weeks of paperwork, and may prevent the need for a full formal appeal.

Step 6: Write a Strong Appeal Letter
A well-crafted appeal letter can make all the difference. Make it concise, factual, and persuasive.
Include:
- Patient and claim info: Name, DOB, insurance ID, prior authorization/claim number, and dates of service.
- Denial details: Reference the denial reason and include denial codes or insurer terminology.
- Medical necessity justification: Explain why the treatment is essential, citing clinical guidelines, research, and physician letters.
- Supporting documentation: Attach clinical notes, lab reports, referrals, and prior authorizations.
- Request and outcome: Clearly state what you want approved and mention any urgency.
- Contact info: Name, phone, and email of the provider or representative filing the appeal.
Need to file an appeal fast? Don't start from scratch.Download the free Appeal Letter Template PDF
Step 7: Submit Through the Correct Channel
Submitting through the right channel ensures your appeal isn’t delayed or rejected.
Tips:
- Check if your insurer requires a specific form or email/fax submission.
- Keep a copy of everything you send.
- Confirm receipt with the insurer to avoid lost documentation.
Step 8: Follow Up Regularly
Don’t just wait, proactive follow-up improves your chances of success.
What to do:
- Call the insurer to confirm the appeal is in process.
- Track decision timelines and escalate internally if delays occur.
- Keep a record of all communication, including dates, names, and summaries of conversations.

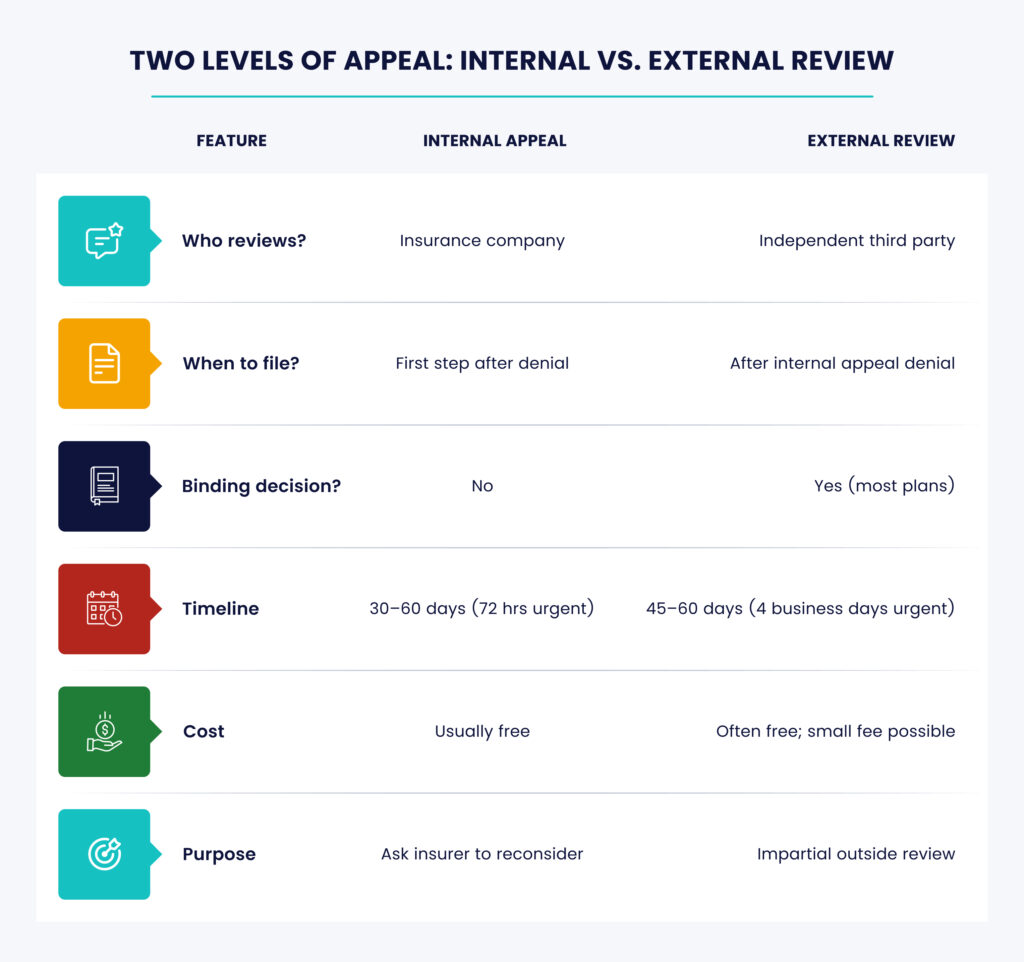
Step 9: Escalate if Needed – Request an External Review
If the internal appeal is denied, you can request an external review by an independent third party.
Key Points:
- The insurer must abide by the reviewer’s decision.
- External reviews are usually state- or federally regulated.
- Filing fees, if any, are often capped or waived.
External reviews cover:
- Medical necessity
- Appropriateness of care
- Level or setting of care
- Experimental treatment determinations
- Surprise billing or cost-sharing disputes
Who can help with prior authorization appeals? Your provider, experienced medical billing staff, or RCM virtual assistants (VAs) can guide you through the appeal process, organize your documentation, and ensure nothing is missed. Having the right support can make the process faster and more effective.
Why Prior Authorization Requests Get Denied

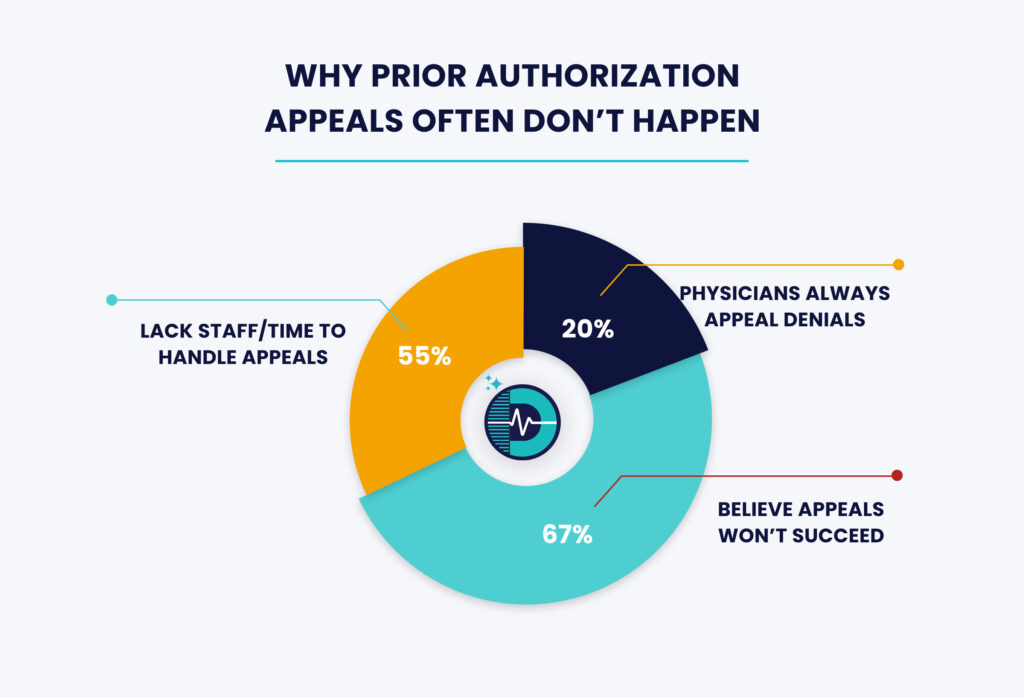
Why Prior Authorization Appeals Often Don’t Happen
According to an AMA Study:
Two Levels of Appeal: Internal vs. External Review
What Kinds of Denials Can Be Appealed?
Most prior authorization denials can be appealed. This includes medical necessity, coverage, out-of-network, experimental treatments, and post-service reimbursements. Even denials that seem final can often be reversed with complete documentation and timely submission.
Gold Carding & the WISeR Model: 2026 Updates for Prior Authorization
In 2026, prior authorization is evolving to make healthcare more efficient and reduce administrative burdens. Two key developments: Gold Carding programs and the WISeR (Wasteful and Inappropriate Service Reduction) Model are helping providers streamline approvals while improving patient care.
| What Is Gold Carding? | The WISeR Model |
| Gold Carding recognizes providers who consistently submit accurate, complete, and guideline-aligned PA requests. High-performing practices may be exempt from certain PA requirements, which: 1. Speeds up patient care 2. Reduces administrative work 3. Protects revenue 4. Highlights compliance and quality performance | WISeR is a voluntary initiative targeting wasteful or low-value services in Medicare. It combines: 1. AI & Machine Learning to analyze PA requests efficiently 2. Human clinical review to ensure medical necessity By focusing on services prone to overuse, WISeR helps providers achieve timely, evidence-based approvals and maintain high performance. |
How Providers Can Benefit
Providers with 90%+ PA approval rates and evidence-based documentation practices are most likely to qualify for Gold Card exemptions. Leveraging WISeR-supported tools helps:
- Avoid unnecessary denials
- Ensure submissions meet payer expectations
- Optimize clinical and administrative workflows
Summary: Gold Carding and WISeR represent positive changes in prior authorization. They reward high-performing providers, reduce administrative barriers, and support timely, evidence-based patient care.
How to Prevent Prior Authorization Denials Before They Happen

Stay Up to Date on Prior Authorization Improvements with Dastify Solutions
Learn More About PA
Final Takeaway: A Denial is a Delay Not a Dead End
If insurance denies your patient’s treatment, you still have options. With the right steps, documentation, and follow-up, many denials can be overturned. But if denials are becoming routine, the sooner you fix the PA process, the sooner you protect patient care and revenue.
Looking for help with prior authorizations? 98% first-pass approvals and 72-hour urgent case turnaround. Get Expert PA Support →