Serving hepatology practices with 500+ certified billers across 50+ specialties, we cut A/R days to 20–30 and maximize reimbursements.
With a team of trained billers and AAPC/AHIMA-certified coders, every claim is handled with clinical depth. Even minor errors are caught before they impact revenue, helping practices reduce denials by 35–40% and increase collections by up to 20%.
How We Solve It
Our integrated hepatology and gastroenterology billing outsourcing solutions reduce these fears with predictable workflows, clinical-depth coders, and automated denial prevention.
If you’ve ever stared at a denial thinking, “What now?” you’re not alone. Common trouble spots include:
Complex Procedures
Shared GI Procedures
Screenings & Specialty
Programs
Denial Codes That Hit Hepatology Hardest
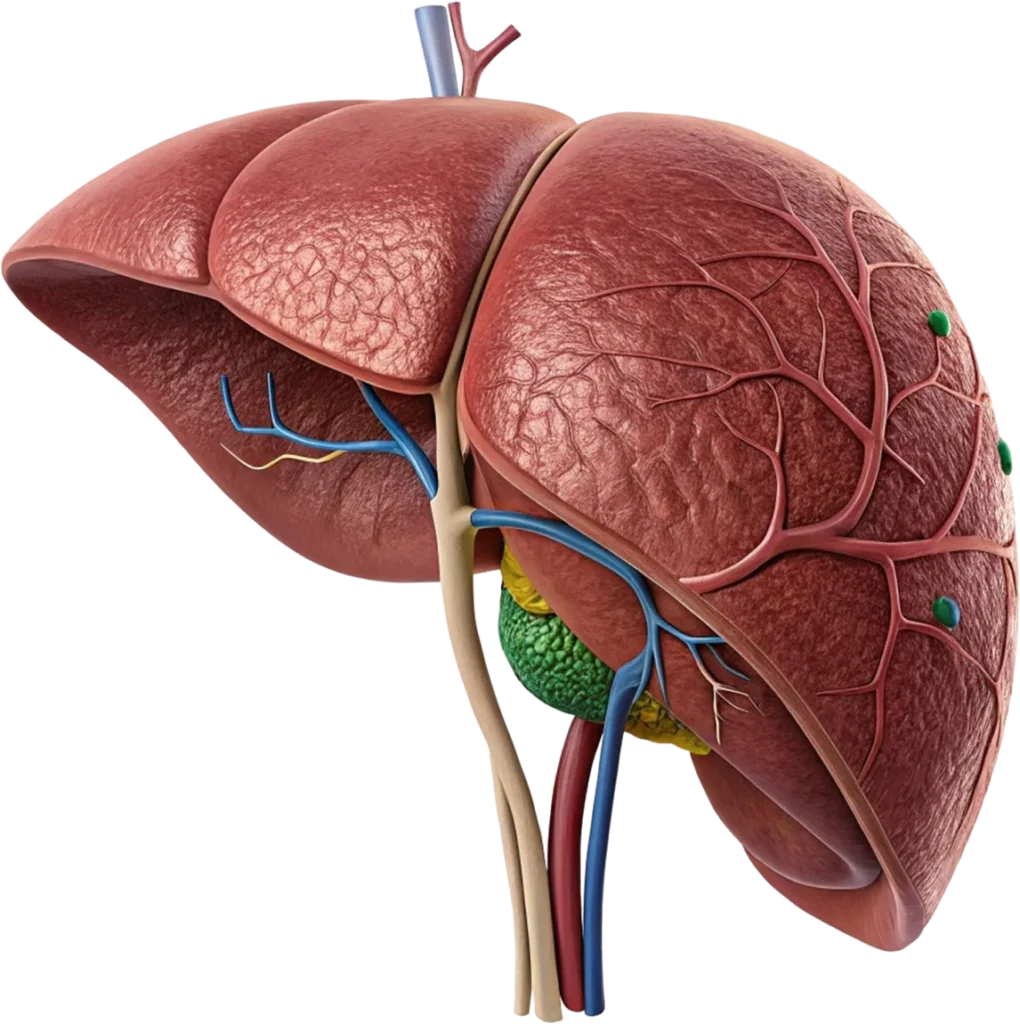
Liver Disease Billing & Coding
Hepatitis & Specialty Drug Billing
Liver Transplant Billing Specialists
Gastroenterology and Hepatology RCM Integration
EHR-Integrated Hepatology Billing Services
Hepatology Billing Automation and Denial Management
Insurance Verification & Claims Submission
H. Patient Financial Experience
Connect with 600+ EHR systems in 1–2 days; no system switch required.
Documentation reviewed by AAPC/AHIMA-certified coders familiar with hepatology.
Scrubbed and QA-checked within 72 hours.
DSO drops below 35 days after the first month.
Keep A/R >90 days under 10%.
Track coding accuracy, underpayments, denials, transplant case summaries, and value-based care performance.

FAQs: Still Have Questions?